Salvinorin A. Is it possible to have a truly powerful painkiller that is not addictive?
We need new drugs. The opioid epidemic gripping the United States has brought into public awareness a problem that has bedeviled the world of medical science for decades: is it possible to have a truly powerful painkiller that is not addictive?

Psymposia is a 501(c)(3) nonprofit research and media organization that offers critical perspectives on drugs, politics, and culture. We rely on contributions from our readers and listeners. Your support is vital to sustaining Psymposia.
Support Psymposia’s independent journalism on Patreon and help us drive the Mystery Machine! We’re a bunch of meddling kids who are unmasking the latest shenanigans on the psychedelics beat.
The opioid epidemic gripping the United States has brought into public awareness a problem that has bedeviled the world of medical science for decades: is it possible to have a truly powerful painkiller that is not addictive?
The simple, unfortunate fact is that the most effective pain medications currently known to science can be both addictive and, when used incorrectly, lethal. While experts and pundits may go back and forth on who exactly gets addicted and why (not to mention the ongoing debate about what it means for something to be addictive, and what addiction really is, anyway), and doctors have successfully found ways to reduce the risks inherent in opiate use, the fact remains that painkillers can be a risky business. A meta-analysis of studies of patients prescribed opioids for chronic pain found that between 8 and 11 percent met the clinical criteria for addiction. For patients given short-term courses of opioids to control acute pain, the rates are much, much lower. The American Society for Addiction Medicine estimates that approximately 23 percent of those who use heroin develop a dependency. As long as opium has been known, the bitter irony has always been that the drugs most effective for easing pain can create so much of it themselves.
While other, non-opioid painkillers do exist (as anyone who’s ever taken an ibuprofen for a headache knows), and can be incredibly useful for mild to moderate pain, it is an unfortunate fact that they are rarely suitable for extreme cases, when pain relief is needed most. I was once hospitalized for a 1cm-wide kidney stone, and no amount of Advil could compare to the stopping power of an intravenous shot of Dilaudid (a powerful, opioid analgesic also known as hydromorphone, which the attending nurse memorably referred to as ‘happy juice’). The need for a powerful but non-addictive pain reliever remains a glaring gap in the Western medical cannon. Some doctors and researchers think that it might be impossible, and pain relief will always be inextricably linked to addictive potential.
As is so often the case, when modern medicine fails to deliver (which it still does, despite the amazing successes of medical science), the eyes of both patients and researchers turn to the natural world: plants have been conducting organic synthesis for millions of years and are far more creative and adept at it than humans are. Very often Indigenous cultures have found different plants and incorporated their healing properties into their own pharmacopoeias. Often times this knowledge is taken by scientists and the medicinal plants are studied and new pharmaceuticals are derived, which would have remained unknown if not for the initial Indigenous discoveries. There is a deep and complex conversation about colonialism, and specifically science’s role in perpetuating colonialist attitudes. For many, the combination of natural evolution and Indigenous knowledge have provided relief from suffering when rational drug design fails to deliver.
So has any culture, anywhere, found something like a powerful, non-addictive, natural painkiller?
The Mazatec People & Salvia’s Historical Use
Amazingly, yes: Salvia divinorum, most well-known as the herb that reliably triggers miserable trips when smoked, has been used as a medicine and a painkiller for hundreds of years by the Indigenous people of Mexico’s Oaxaca region. While individual U.S. states have banned it (29 in all, including the territory of Guam), the federal government has, somewhat surprisingly, continued to ignore Salvia divinorum and kept it off the list of controlled substances.
Anthropologists working among the Mazatec people of Oaxaca, Mexico have known for decades that the Salvia divinorum plant plays an important role in Mazatec culture and medicine. Rather than smoking it (which is the preferred route of administration in the United States, which Mazatec shamans have apparently objected to), it is normally administered as a quid: leaves are chewed and swallowed rather than smoked or boiled (although there are records of infusions being made). While the psychic effects are still clearly present, and considered to be spiritually significant, salvia is used for far more than altering consciousness: it has also been used as a pain-reliever (headaches in particular were noted as being responsive to salvia) and to alleviate gastrointestinal upsets and problems associated with alcoholism. Unlike morphine-based pain remedies popular in the West, within the Mazatec culture, there is little evidence that Salvia divinorum is used recreationally or that anyone is becoming dependent on it. A survey by Erowid of Western Salvia divinorum users found similar results: addiction to salvia is largely unheard of.
While Western anthropologists had known about the psychoactive effects of Salvia divinorum since the early 20th century, the active molecule was not isolated and identified until 1983 by Ortega et al., in Mexico, and it wasn’t until 1993 that the unique receptor profile of Salvia divinorum was understood. Perhaps because of its unique and often unpleasant effects, and despite being known to such psychedelic luminaries as Gordon Wasson and Albert Hoffman (a popular strain of the Salvia divinorum plant is named Hoffman-Wasson after the pair), Salvia divinorum did not enter the popular consciousness in the same way that LSD, psilocybin, and mescaline did in the mid-20th century.
The Science of Salvia
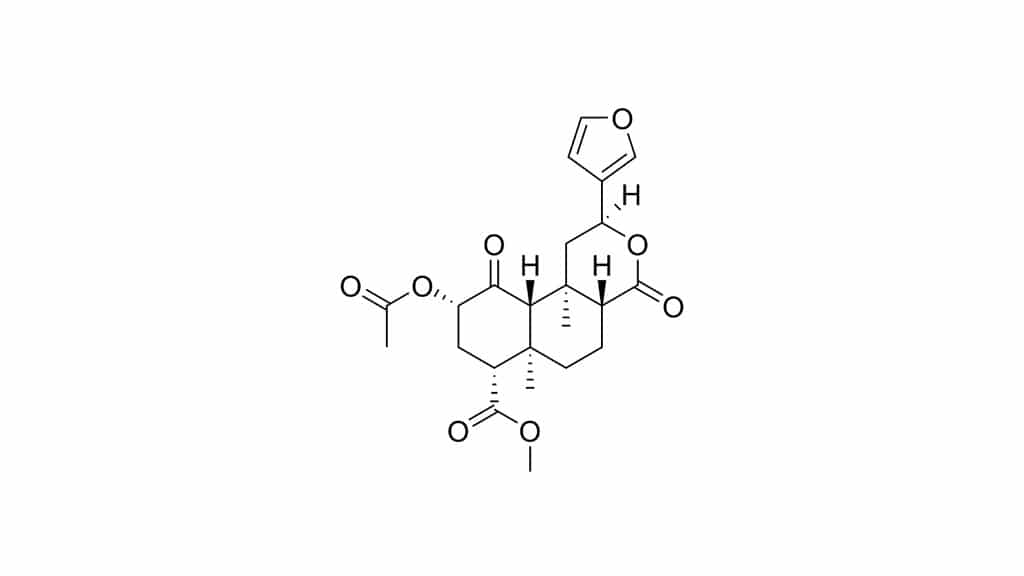
So what do we know about Salvia divinorum’s pain-relieving properties? The active compound in any preparation of the plant is a molecule called Salvinoin-A, which is almost unique among psychedelic drugs in that, while almost all other psychedelics work by activating some combination of serotonin and dopamine receptors, Salvinorin-A has an affinity for the somewhat-obscure opioid receptor: the kappa-opioid receptor (usually abbreviated as the KOR), which, as far as we know, is not targeted by any other commonly-used drug. Unlike a plant like cannabis, which has thousands of individual molecules that synergize to create its effect, Salvia divinorum’s effects come exclusively from Salvinorin-A. While metabolites similar to Salvinorin-A have been isolated from the plant, none of them appear to have appreciable psychoactive effects (although synthetic derivatives have been created that show comparable effects).
In a very simplified sense, the kappa-opioid receptor can be thought of as the opposite twin of the more well-known mu-opioid receptor, which is what drugs like morphine target. Together, they seem to perform a balancing act that is integral to our own innate ability to learn. The mu-opioid receptor mediates ‘rewards.’ Behaviors that trigger its activation (like having sex, eating a good meal, or shooting a bunch of heroin), result in feelings of well-being and euphoria, which can become addictive. The brain learns to do whatever it is that triggers the mu-opioid receptor. The kappa-opioid receptor, on the other hand, seems to do the opposite. Stimuli that triggers that receptor and the feelings created are of stress, dysphoria and aversion. There are other interesting symmetries: mu-opioid receptor agonists cause itching while kappa-opioid receptor agonists suppress it. Taking something like salvia with something like heroin also seems to blunt the effects of both drugs, which is what you would expect to see if the mu and kappa opioid receptors worked in opposition. Together they help us navigate complex environments full of both rewarding and aversive behaviors, and when everything is working smoothly, they balance one another out. They both, however, seem to dull pain.
The pain-killing effects first discovered by the Mazatec people have borne out under scientific scrutiny. In a series of somewhat heart-breaking studies, scientists took rats and mice and subjected them to a battery of ways to induce pain, which range from putting them on hot-plates that burn their feet, to shooting their tails with lasers, both with and without infusions of Salvinorin-A. Across the board, the mice that were treated with Salvinorin-A showed fewer signs of experiencing pain. The effect is clear: Salvinorin-A is an effective analgesic. In fact, it’s very effective: it’s active at extremely low doses (200ug, making it one of the strongest known, naturally occurring psychoactive compounds) and doesn’t seem to have any point of lethal overdose, unlike opiate painkillers, where high potency usually translates into increased risk of death. Even chronic exposure to high doses doesn’t do damage to vital organs.
The non-addictive nature observed by anthropologists and user-surveys has also been validated by animal studies. The usual tests for addictiveness indicate that Salvinorin-A is extremely unlikely to be addictive. It may even have anti-addictive properties: beyond simply not having effects seen as indicative of addictive potential, Salvinorin-A has been found to exhibit the opposite effect. For example, almost all addictive drugs increase the amount of dopamine activity in a brain region called the nucleus accumbens. Salvinorin-A not only fails to increase dopamine in this region, it seems to actively suppress it. Similarly, in tests of addictive drugs, many animals will show ‘conditioned place preference,’ frequently returning to areas where they received infusions of the drug, even when they’re not receiving any. Salvinorin-A has the opposite effect, creating ‘conditioned place aversion.’ As with the pain-relieving properties, the evidence is clear: Salvinorin-A (and by extension Salvia divinorum) is unlikely to have the same addictive qualities that can make opiate painkillers dangerous. Drugs like Salvinorin-A have even shown promise as a treatment for addiction to other substances, including cocaine and alcohol.
So, thus far, we have a powerful, non-addictive painkiller that is physiologically safe, with no known lethal overdose effect. So what’s the problem? Why aren’t we getting Salvinorin-A infusions in hospitals?
Why It’s Not A Great Medicine
While Salvinorin-A does have some extremely appealing properties, there are a few things that make it completely unsuitable for use as a replacement for our current pain medications. One is that it is only active for a brief period. Anyone who’s smoked Salvia knows that a user will only be under the influence for a few minutes, and even when administered as a quid, the effect doesn’t last longer than an hour. While short-acting pain-killers can be useful in surgery (fentanyl being one famous example), for extended pain management, they leave much to be desired. The other negative, which is something of an elephant in the room, are the hallucinations.
The effects of Salvinorin-A when rapidly administered (such as smoking or injection), or administered in high doses have the potential to be extremely unpleasant. The ‘trip reports’ section of Erowid’s Salvia divinorum vault is full of experiences that range from mildly-distressing, to traumatically disturbing (one that sticks out in my memory is one of a young man who smoked it and felt himself become part of some kind of cosmic machine made of meat). While experienced psychonauts may be able to manage these experiences with appropriate preparation and knowledge, a hospital is possibly one of the worst places to experience a profound and florid psychosis. Earlier I mentioned being given an i.v. of Dilaudid while in the hospital for kidney stones, and I cannot imagine how awful it would have been to have my painkiller also serve as a ticket to Cthulhu’s birthday bash. Such experiences are hard enough in a normal frame of mind, and as far as sets and settings go, being scared, vulnerable, and in pain seem like the worst possible place to embark on a psychic journey.
Looking Forward: What We Can Learn From Salvia
Does that mean we’re done? Decades of research (not to mention a few minutes of your life) tossed in the bin? Not at all. While Salvinorin-A may not make its way into a medical setting, this research has generated a tremendous amount of new data which can be used to start looking for drugs similar enough to Salvinorin-A to take advantage of the positive effects. We now know that selective kappa-opioid receptor agonists are physically safe, effective pain-killers with low addictive potential.
From here there are many directions research can go. There has been some evidence of analogues of Salvinorin-A that cannot cross the blood-brain-barrier (and therefore cannot cause strange effects to consciousness). Clinical trials of a peripherally selective kappa-opioid receptor agonist called asimadoline have been very promising, especially for irritable bowel syndrome (one of the conditions the Mazatec have been using Salvia divinorum to treat for centuries. Other drugs have been developed that try to combine traditional opiate drugs with kappa-opioid receptor agonists in an attempt to balance the effects and reduce the risk of addiction. While psilocybin, LSD, and ibogaine have recently received significant press for their potentially anti-addictive properties, Salvia divinorum shouldn’t be forgotten and may yet have a role to play in the development of our understanding and treatment of addiction.
For individuals with painful conditions like migraines, or IBS, it is certainly possible that they could take inspiration from the Mazatec people and grow their own medicine. The Indigenous people of the Americas were using it as an effective medicine while European doctors were still debating whether it was a good idea to wash their hands before surgeries, and while simply chewing the raw leaf will have some consciousness-altering effects, some may feel that it’s a worthwhile trade-off.
Sometimes there can be a feeling that psychedelic research must necessarily lead to the legalization or prescription of the drug in question. The research into cannabis, psilocybin, MDMA, ibogaine, and LSD are all currently aimed at bringing these compounds into a Western medical framework so that they might one day be prescribed by doctors in white lab coats. There is another side of psychedelic research that is decidedly less glamorous but just as important: doing basic research on Salvia divinorum and Salvinorin-A may never result in someone filling a prescription for salvia at the local CVS, but the things we learn may help change the face of medicine.
Hey! Before you go… Psymposia is a 501(c)(3) non-profit media organization that offers critical perspectives on drugs, politics, and culture. We strive to ask challenging questions, and we’re committed to independent reporting, critical analysis, and holding those who wield power accountable.
Our perspectives are informed by critical analysis of the systemic crises of capitalism that have directly contributed to the unmitigated growth of addiction, depression, suicide, and the unraveling of our social relations. The same economic elite and powerful corporate interests who have profited from causing these problems are now proposing “solutions”—solutions which both line their pockets and mask the necessity of structural change.
In order for us to keep unpacking these issues and informing our audience, we need your continuing support. You can sustain Psymposia by becoming a supporter for as little as $2 a month.
Thomas Varley
Thomas Varley has a BA in Neuroscience from Hampshire College, and studies Clinical Neuroscience at University of Cambridge.